Hemoglobin A1C (HbA1c): Understanding Your Diabetes Management
Explore Hemoglobin A1C (HbA1c) to better manage diabetes and improve your overall health.

Super Health Lab Key Takeaways
Summary: Understanding Hemoglobin A1C (HbA1c) is essential for effective diabetes management:
- 🩸 HbA1c measures average blood sugar levels over time, typically reflecting the past two to three months. This assessment helps in understanding long-term glucose control in diabetes management.
- 📊 Regular testing of HbA1c is crucial for monitoring diabetes progress. It assists healthcare providers in adjusting treatment plans and medications for optimal blood sugar stabilization.
- 🍏 Lowering HbA1c levels can significantly reduce the risk of diabetes-related complications. Targeting specific HbA1c goals can improve overall health and well-being for diabetic individuals.
- 💊 Lifestyle changes, including diet and exercise, can positively influence HbA1c levels. Implementing healthier habits plays a vital role in enhancing diabetes management and improving glycemic control.
- 🗓️ Consulting with healthcare professionals about HbA1c results fosters proactive diabetes care. Collaborative discussions enable better-informed decisions regarding treatment adjustments and lifestyle modifications.
Managing diabetes effectively requires knowing how your blood sugar levels behave over time. If you’ve recently been diagnosed with diabetes or are working to stay on top of your health, you’ve likely heard of the Hemoglobin A1C (HbA1c) test. But what exactly is HbA1c, and why is it so important? Whether you're newly diagnosed, managing prediabetes, or supporting a loved one, understanding the role of HbA1c can empower you to make better decisions for long-term health. In this guide, we'll break down what the HbA1c test measures, how it impacts diabetes management, target goals, and practical ways to improve your numbers. Let’s explore how this essential health marker fits into your wellness journey.
What Is Hemoglobin A1C (HbA1c) and Why Does It Matter?
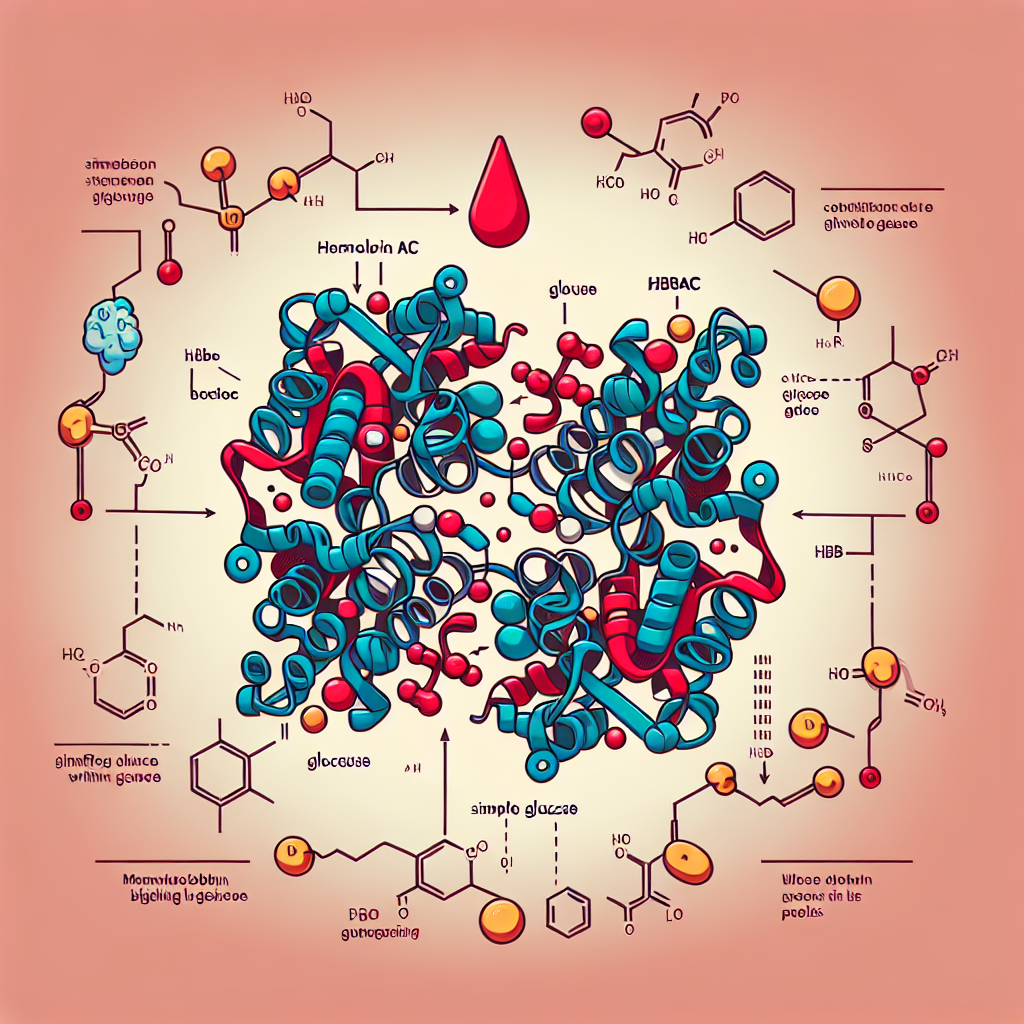
Hemoglobin A1C (often abbreviated as HbA1c or simply A1C) is a blood test that measures the average level of blood sugar (glucose) over the past two to three months. Specifically, it looks at the percentage of hemoglobin—a protein in red blood cells that carries oxygen—that is coated with sugar (glycated). Because red blood cells have a lifespan of about 120 days, the HbA1c test offers a longer-term picture of blood sugar control than daily monitoring.
A normal HbA1c level is below 5.7%. A reading between 5.7% and 6.4% indicates prediabetes, while a level of 6.5% or higher usually signals diabetes.
Understanding HbA1c matters because it directly correlates with your risk of developing diabetes-related complications. Elevated HbA1c levels are linked to cardiovascular disease, nerve damage, kidney failure, and vision problems. This makes the A1c test an essential tool not just for diagnosis but also for ongoing management.
Unlike a simple blood sugar check, the HbA1c test isn't affected as much by short-term factors like meals or stress. It provides a broader view of how well you're managing your diabetes, helping both you and your healthcare team make informed treatment decisions. Many health organizations, including the American Diabetes Association (ADA), recommend that people with diabetes check their HbA1c levels two to four times a year depending on their treatment plan and how well they are meeting their goals.
How Is the HbA1c Test Done and Interpreted?
Getting your HbA1c tested is straightforward. It's typically a simple blood draw conducted at a lab or healthcare setting. Some clinics offer point-of-care testing, where a sample from a finger prick provides immediate results within minutes.
After collection, the blood sample is analyzed to determine the percentage of glycated hemoglobin. The final number you receive reflects the average blood glucose over the preceding two to three months in percentage form. Here's how to interpret common results:
- Below 5.7%: Normal blood sugar range.
- 5.7% - 6.4%: Prediabetes; higher risk of developing diabetes.
- 6.5% and above: Diabetes diagnosis.
- Less than 7%: General target for many adults with diabetes, as recommended by organizations like the ADA.
However, targets can be personalized. For instance, younger individuals without significant health issues may aim for stricter control (HbA1c closer to 6.5%), whereas older adults or those with comorbid conditions might have a higher target to reduce the risk of hypoglycemia.
It's important to note that certain factors can affect HbA1c accuracy. Conditions that alter red blood cell lifespan—such as anemia, kidney disease, or recent blood loss—can skew results. Other variables, like ethnic background and the specific laboratory method used, may also have minor effects.
Modern A1C tests now standardize results according to the National Glycohemoglobin Standardization Program (NGSP) criteria, helping ensure consistency across different laboratories. As always, your healthcare provider will interpret results in the context of your overall health and history.
Setting HbA1c Goals for Effective Diabetes Management
Once an HbA1c result confirms a diagnosis or current status, the next step is establishing personal goals. Maintaining a controlled HbA1c level reduces the likelihood of long-term complications and enhances quality of life.
For most adults living with diabetes, the target HbA1c is set below 7%. The ADA suggests this benchmark based on solid evidence that tight glycemic control decreases risks like neuropathy, eye diseases, and cardiovascular events. However, ideal targets are individualized based on several factors:
- Age and Life Expectancy: Younger patients may benefit from stricter glucose control, whereas older adults may prioritize avoiding lows (hypoglycemia) rather than aiming for very tight control.
- Duration of Diabetes: Someone newly diagnosed might achieve lower HbA1c numbers more safely than someone who has had diabetes for decades.
- Presence of Complications: If complications like heart disease or kidney problems are already present, moderate targets can balance the risks and benefits more effectively.
- Risk of Hypoglycemia: Frequent low blood sugar episodes may necessitate a slightly higher target to preserve safety.
For example, a 22-year-old college student recently diagnosed with type 1 diabetes might aim for an A1c of 6.5%, while a 75-year-old with heart disease might be better off maintaining an A1c around 7.5% or even slightly higher.
Critical to achieving and maintaining these goals is regular monitoring, consistent communication with healthcare providers, and lifestyle adjustments such as diet, exercise, medication adherence, and mental health support. In some cases, continuous glucose monitoring (CGM) systems can supplement HbA1c tracking by offering real-time data on blood sugar fluctuations.
Hemoglobin A1C (HbA1c) is a crucial blood test that measures average blood sugar levels over the past 2 to 3 months, providing essential insights for diabetes management. Maintaining HbA1c levels below 7% is generally recommended for most adults to minimize complications associated with diabetes, such as heart disease, kidney damage, and nerve issues. Regular monitoring allows for timely adjustments in treatment, significantly improving long-term health outcomes. Understanding your HbA1c levels is vital for effective diabetes control and overall well-being.
Practical Strategies to Improve Your HbA1c Levels
Improving your HbA1c isn't about quick fixes—it's about sustainable, informed changes that promote balanced blood glucose over time. Here are effective, practical strategies for better A1c outcomes:
Nutrition Optimization
Choosing whole, unprocessed foods benefits blood sugar control significantly. Focus on fiber-rich vegetables, lean proteins, healthy fats, and whole grains. Limit simple carbs, sugary beverages, and overly processed foods. For example, swapping white rice for quinoa and drinking water instead of soda can make a noticeable difference over weeks and months.
Consistent Physical Activity
Exercise helps your body use insulin more effectively, lowering blood sugar naturally. Aim for at least 150 minutes of moderate aerobic activity per week—like brisk walking, cycling, or swimming. Resistance training two to three times a week enhances muscle mass, further aiding glucose metabolism.
Medication Adherence
For those who take medications (such as metformin, insulin, or newer injectable options like GLP-1 receptor agonists), following your prescribed regimen is crucial. Skipping doses or inconsistent use can lead to erratic blood sugar levels and elevated HbA1c.
Monitoring and Feedback Loops
Regular home blood sugar checks—even if infrequent—help spot trends. Devices like continuous glucose monitors (CGMs) provide valuable insights into how lifestyle choices affect your blood sugar. Sharing this data with your healthcare provider allows you to fine-tune your management plan.
Stress Management and Sleep Hygiene
Chronic stress and insufficient sleep can raise blood sugars. Techniques such as mindfulness, meditation, cognitive behavioral therapy, and establishing a stable sleep schedule (7-9 hours nightly) can support healthier numbers.
Consider small habit changes: adding one vegetable to every meal, taking a 10-minute walk after dinner, or setting a phone reminder for medication. Every little step adds up, often leading to noticeable changes in HbA1c within 3 to 6 months—the typical life cycle of red blood cells.
Understanding and managing your Hemoglobin A1C (HbA1c) is a cornerstone of effective diabetes care. This simple blood test offers critical insights into your average blood sugar levels over time, reflecting the success of your current management strategies and guiding future adjustments. Knowing your target A1c range—and working systematically toward it through tailored lifestyle changes, medication adherence, and continuous monitoring—can dramatically improve your overall health outcomes.
While the journey requires consistency and support, each improvement in your HbA1c percentage represents a meaningful step toward a healthier future. Partner with your healthcare provider, stay informed, and celebrate the progress you make along the way. By keeping your HbA1c in check, you’re not just managing diabetes—you’re actively building a brighter, healthier life.
Frequently Asked Questions
HbA1c levels reflect a person's average blood sugar levels over the past two to three months. This information is crucial for managing diabetes, as it helps healthcare providers assess how effectively blood sugar levels have been controlled and to make necessary adjustments in treatment.
Generally, an HbA1c level below 5.7% is considered normal, while levels between 5.7% and 6.4% indicate prediabetes. A level of 6.5% or higher on two separate tests usually confirms a diabetes diagnosis. Monitoring these levels aids in preventing complications associated with high blood sugar.
HbA1c testing is crucial for diabetes management as it provides a comprehensive overview of glucose control over time, unlike daily blood sugar tests that only show short-term levels. This long-term average helps in evaluating the effectiveness of treatment plans, dietary habits, and lifestyle modifications.
Additionally, understanding HbA1c results allows for timely adjustments to medications or lifestyle changes to prevent complications such as cardiovascular disease, kidney damage, and nerve issues that can arise from poorly managed diabetes.
The frequency of HbA1c testing can vary based on individual circumstances. For those with stable blood sugar levels and controlled diabetes, it is usually recommended to test every six months. However, if adjustments to medications are made or if blood sugar levels fluctuate, testing every three months may be advisable.
Regular testing helps ensure that any changes in health or treatment efficacy are promptly identified and addressed, contributing to better overall diabetes management and reduced risks of complications.
Several factors can influence HbA1c levels, including overall blood sugar control, the lifespan of red blood cells, and certain health conditions. For instance, conditions such as anemia or kidney disease can affect red blood cell turnover, thus skewing HbA1c results.
Additionally, factors such as recent illness, stress, and hormonal changes can also impact glucose levels and, consequently, HbA1c measurements, highlighting the importance of a thorough clinical context when interpreting results.
To lower high HbA1c levels, individuals should focus on lifestyle modifications like adopting a balanced diet rich in whole grains, fruits, and vegetables while reducing processed sugars. Regular physical activity significantly contributes to improved insulin sensitivity, helping to manage blood sugar levels.
Moreover, medication adherence, regular monitoring of blood glucose, and collaboration with healthcare professionals are essential in creating an effective management plan. Implementing these strategies collectively aids in lowering HbA1c and enhancing overall health.










